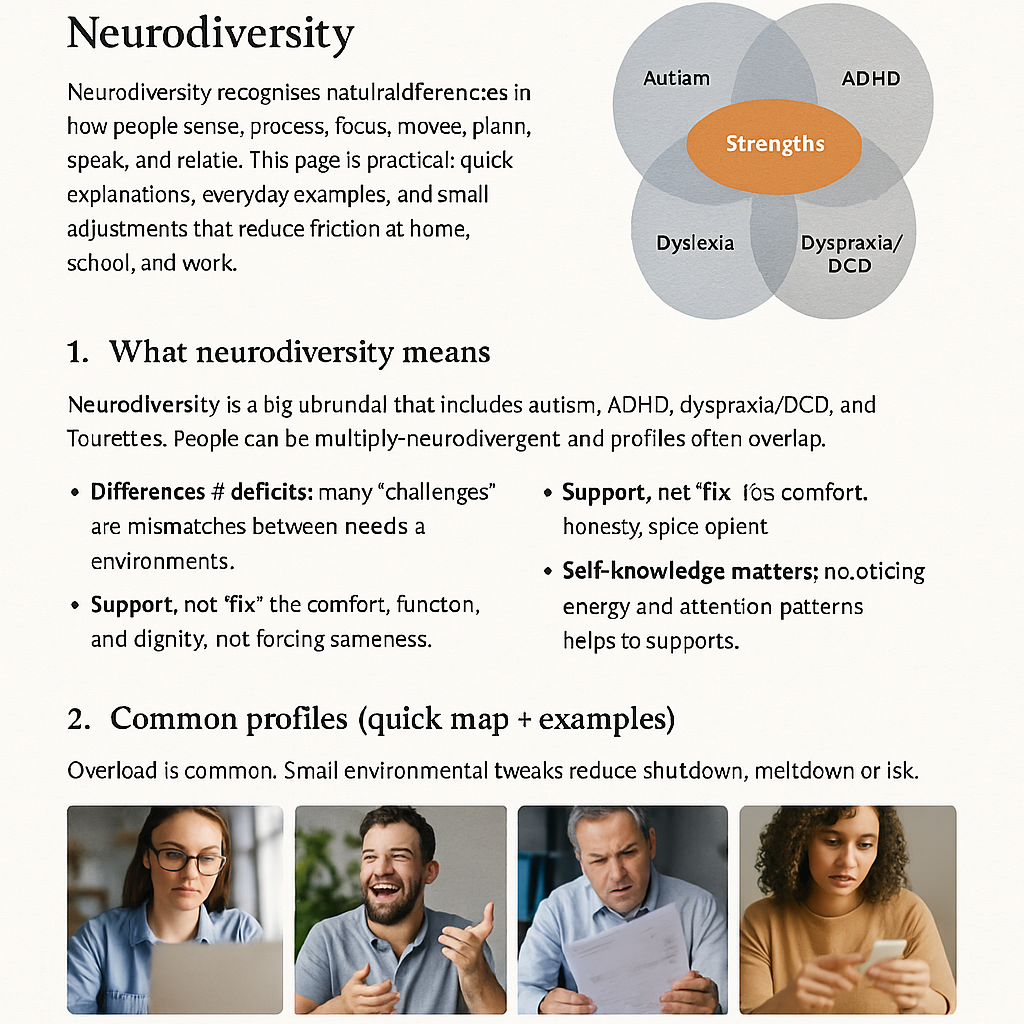
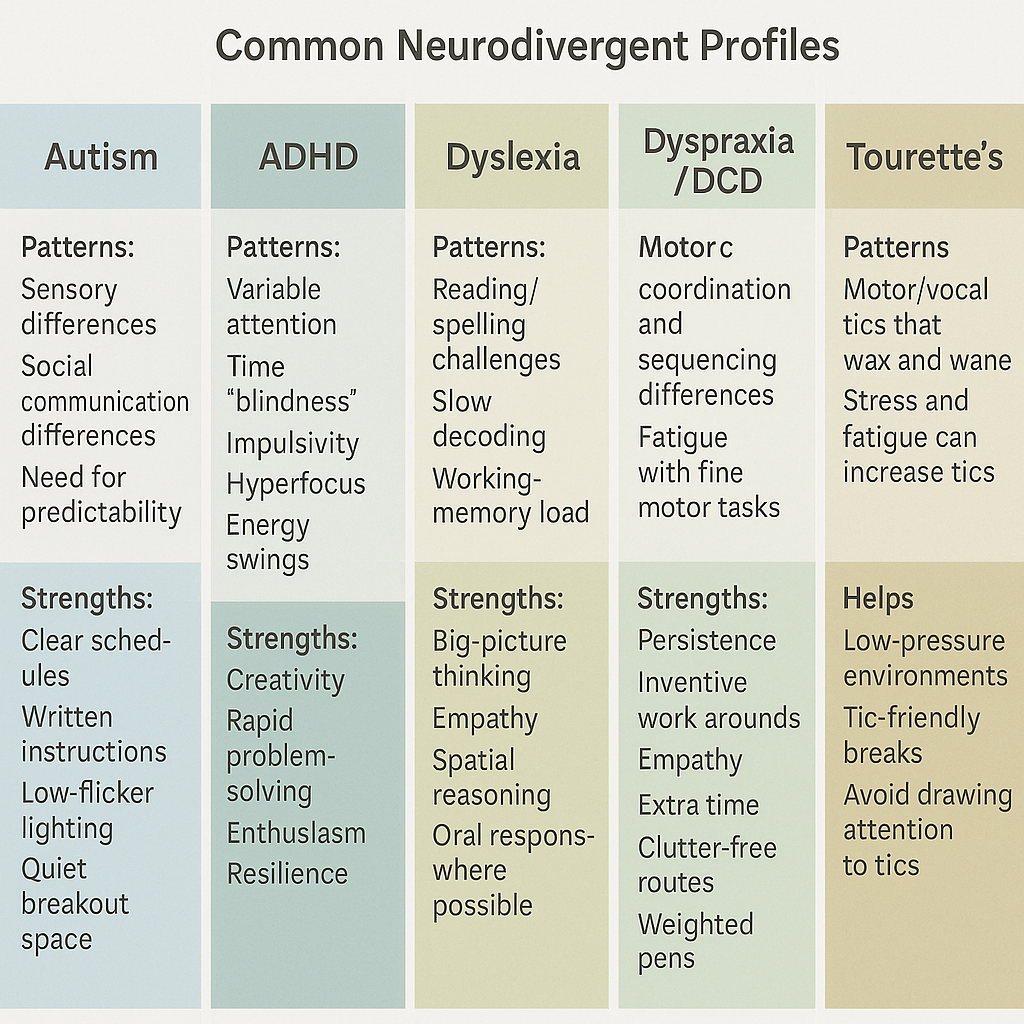
Autism
Patterns: sensory differences; social communication differences; need for predictability; intense interests.
Strengths: deep focus, honesty, specialist knowledge, pattern spotting.
Helps: clear written schedules; concrete instructions; low-flicker lighting; quiet breakout space.
Example: A predictable morning sequence and a visual checklist reduce start-of-day overwhelm.
ADHD
Patterns: variable attention, time “blindness”, impulsivity, hyperfocus, energy swings.
Strengths: creativity, rapid problem-solving, enthusiasm, resilience.
Helps: visual timers; body-doubling; 2–5 minute “gateway steps”; movement breaks; novelty.
Example: “After I put the kettle on, I write 2 lines.” Tiny anchor beats big intentions.
Dyslexia
Patterns: reading/spelling challenges; slow decoding; working-memory load.
Strengths: big-picture thinking, empathy, spatial reasoning, story sense.
Helps: reader-friendly fonts; audio options; mind-maps; oral responses where possible.
Example: Voice-to-text for drafting; a colleague proofreads the final polish.
Dyspraxia / DCD
Patterns: motor coordination/sequencing differences; fatigue with fine motor tasks.
Strengths: persistence, inventive work-arounds, empathy.
Helps: extra time; clear routes; weighted pens; alternative keyboards; rest breaks.
Example: Laptops for notes; fewer transitions between rooms; seated lab tasks.
Tourette’s
Patterns: motor/vocal tics that wax and wane; stress and fatigue can increase tics.
Strengths: humour, creativity, determination.
Helps: low-pressure environments; tic-friendly breaks; avoid drawing attention to tics.
Example: Agree hand signals to pause/continue in meetings; camera-off options.
 Patch & Pot
Patch & Pot