Understanding Depression
Depression isn’t just “feeling sad.” It can flatten energy, numb emotions, and distort thinking. It’s one of the most common mental health experiences worldwide, and in the UK millions live with it every year. Understanding the biology, the daily impact, and the supports available can make it less overwhelming — and remind you that you’re not alone.
1. Understanding Depression
Depression can look like sadness, but also like flatness, irritability, or exhaustion. It affects body, mind, and behaviour:
- Low energy or constant fatigue, even with rest
- Loss of interest or pleasure in things once enjoyed
- Sleep changes: difficulty falling asleep, waking early, or oversleeping
- Appetite changes: eating much less or more
- Negative self-talk: “I’m useless,” “Nothing will help”
- Physical symptoms: aches, slower movements, gut issues
2. Biology / How It Happens
Depression is not a sign of weakness. It reflects changes across several systems in the brain and body.
Neurotransmitters
- Serotonin: regulates mood, sleep, appetite. Low or disrupted signalling is linked with low mood and poor sleep.
- Dopamine: governs motivation and reward. Reduced dopamine makes activities feel unrewarding or joyless (anhedonia).
- Norepinephrine: supports energy and alertness. Low levels can cause fatigue, poor focus, and low drive.
- GABA: the brain’s calming chemical. Low GABA links to anxiety and agitation within depression.
- Cortisol: the stress hormone. In depression, cortisol can stay high, disturbing sleep, memory, and immune function.
Hormones
- Oestrogen & Progesterone: Fluctuations in menstrual cycle, perimenopause, or menopause can destabilise mood and sleep.
- Testosterone: Low levels in men (and women) are linked to reduced energy, drive, and mood.
- Thyroid hormones: An underactive thyroid can mimic depression with fatigue, brain fog, and weight changes.
- Insulin & Blood sugar: Large swings in glucose can cause irritability, fatigue, or brain fog. Stable meals steady mood.
Download Hormones & Mood Guide (A4 PDF)
Lifestyle factors interact with biology:
- Nutrition: balanced meals with protein, complex carbs, and omega-3 fats can support serotonin and dopamine production.
- Exercise: even light daily movement raises endorphins and increases dopamine sensitivity, helping mood lift.
- Sleep: good sleep hygiene (dim light, regular bedtime, no heavy screens late) helps consolidate memory and reset stress systems.
3. Day-to-day coping

- Keep a simple routine: meals, getting dressed, light activity
- Break tasks into tiny steps: “Open laptop” is a task in itself
- Allow rest without guilt — energy is genuinely reduced
- Reach out: text one friend, join a peer group, or write in a journal
4. Support & Connection
Talking with a GP, a counsellor, or a peer group can help you make a plan that fits your life. If face-to-face feels hard, many services offer phone or online options.
5. Hope & Recovery

With the right mix of therapy, support, and sometimes medication, many people recover from depression or learn to manage it so life becomes meaningful again. Small consistent steps matter more than dramatic leaps.
6. Self-talk Upgrades
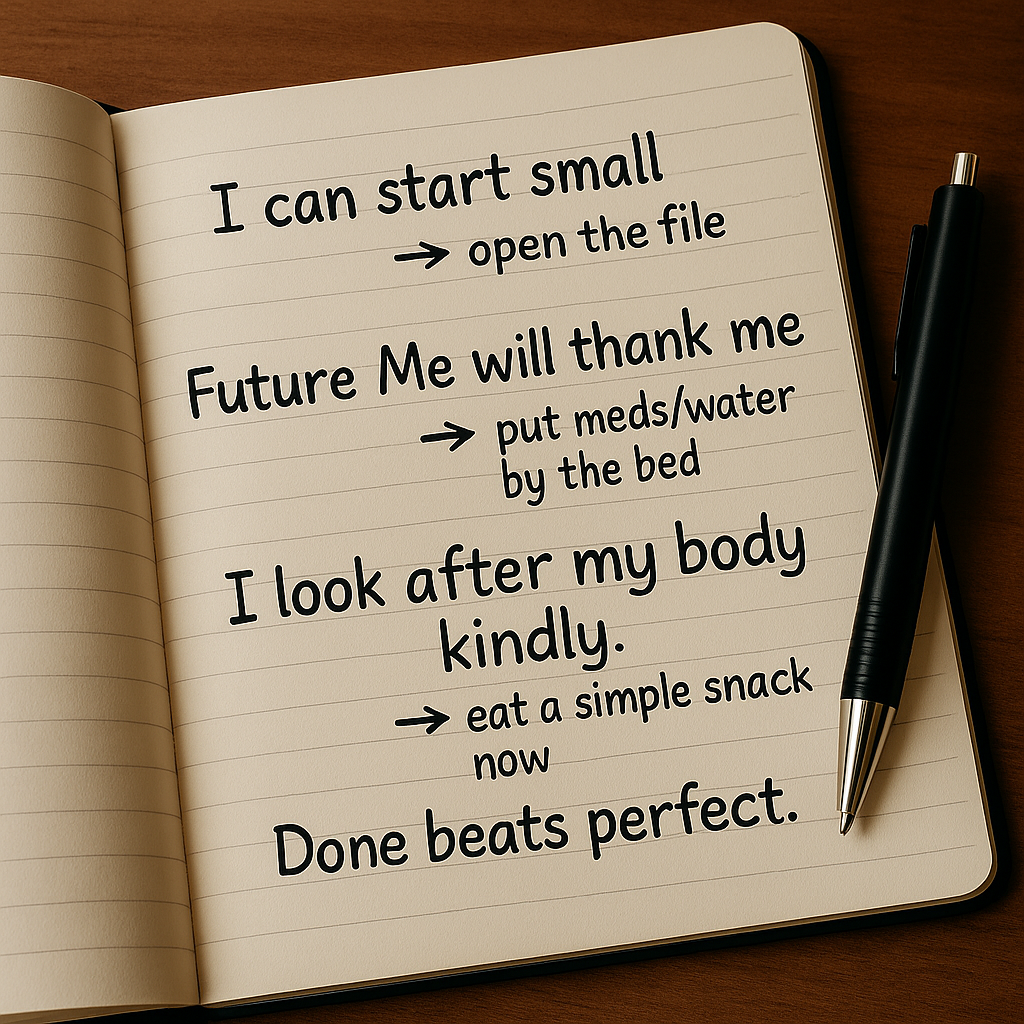
To: “I’m struggling, but still here.”
To: “This feels endless, but feelings shift.”
To: “I can do one tiny step.”
7. Reframes
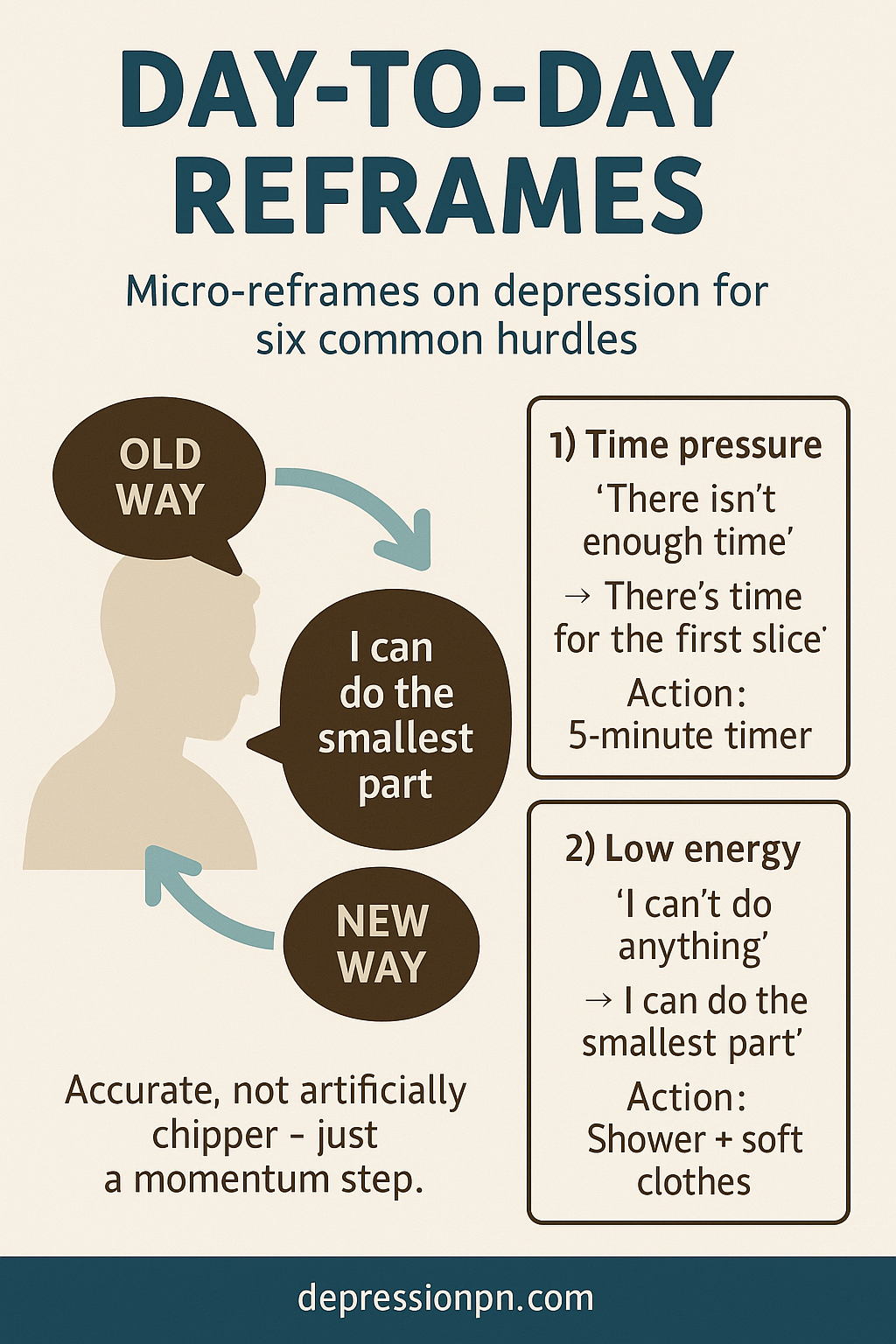
→ “Healing is not linear.”
→ “Needing support is human.”
→ “The brain can adapt over time.”
Important Note
The information on this page is for general understanding and support. It is not a substitute for professional medical, psychological, or legal advice. If you feel unable to keep yourself safe or someone else is at risk, call 999 (UK) immediately. If you’re outside the UK, contact your local emergency number.
For non-emergency concerns, consider speaking with a qualified health professional or one of the support services listed on our site.
 Patch & Pot
Patch & Pot